We are proud to celebrate the achievements of UBC Orthopaedics’ Dr. Babak Shadgan and Dr. Pierre Guy, along with their research team, who have been recognized by the Canadian Orthopaedic Foundation for their research into a patient-first diagnostic testing technique.
Named for Dr. Cy Frank, renowned Canadian orthopaedic surgeon and researcher, the Canadian Orthopaedic Foundation’s Cy Frank Award celebrates and funds excellence in orthopaedic innovation. The Foundation recognizes Drs. Shadgan and Guy for their development of a clinical protocol poised to improve both the patient and practitioner experience during chronic exertional compartment syndrome (CECS) diagnostic testing.
Patients develop CECS when they experience repeated pressure increases in the lower leg. This pressure occurs during exercise and compresses local blood vessels leading to pain, impaired function, and potential tissue damage in the affected area. When individuals with CECS exercise, there is an increase in blood flow and fluid accumulation in the active muscles, which expands against the surrounding fascia, a sheath of connective tissue. CECS can occur in people of all ages, though it is more common among athletes and those with physically demanding jobs.
“Our research has the potential to revolutionize CECS diagnosis, enhancing patient comfort, clinical efficiency, and diagnostic accuracy.” — Dr. Babak Shadgan
Effective management of CECS requires swift and accurate diagnosis to alleviate pain and protect the tissues at risk of damage. However, the current gold standard for CECS diagnosis is both painful and complex to administer. Clinicians must calibrate pressure-sensing needles and place them into each of the four major compartments of the lower leg.

These needles then measure and record intra-compartmental pressure changes before, during, and after the patient exercises, such as running on a treadmill. These results are then analyzed to assess the timing and severity of pressure changes within the compartments. Achieving accurate pressure measurements is time-consuming, technically demanding on the clinician, and uncomfortable for the patient.
Beyond the realities of complex setup and time requirements of traditional CECS testing, there is growing evidence that non-invasive diagnostic tools mitigate some of the factors leading to a delay in patients seeking medical help. By innovating simpler and non-invasive procedures, we are developing a new technique to provide direct benefits to people who are hesitant to seek care due to a fear of pain.
“We are introducing a user-friendly, cost-effective alternative to invasive pressure measurements.” — Dr. Babak Shadgan
Instead of using the invasive needle-and-manometer protocol, the UBC research team devised a means of measuring tissue oxygenation and hemodynamics using near-infrared spectroscopy (NIRS) sensors placed on the compartment’s surface. Because NIRS detects the infrared signatures of target elements, its sensors can determine how far oxygenated blood moves into working tissues and the level of blood oxygenation saturation, offering clinically relevant data on both compartmental pressure and quality of circulation in a non-invasive manner. Further, many risks associated with invasive procedures, like hemorrhage or infection at the needle sites, can be avoided altogether by using technologies located on the skin’s surface.

The research team predicts that the NIRS diagnostic software could have additional applications for other non-invasive diagnostic procedures. The potential for a breakthrough methodology in the diagnosis of CECS places Drs. Shadgan and Guy at the forefront of compartment syndrome research. Dr. Shadgan’s work with NIRS and optical tomography during a Harvard University fellowship establishes him, and this emerging research, as a site of innovation in an area of diagnostic medicine ready to evolve.
“The project addresses the need for a safer and more reliable approach to diagnosing CECS.” — Dr. Babak Shadgan
CECS Research Team
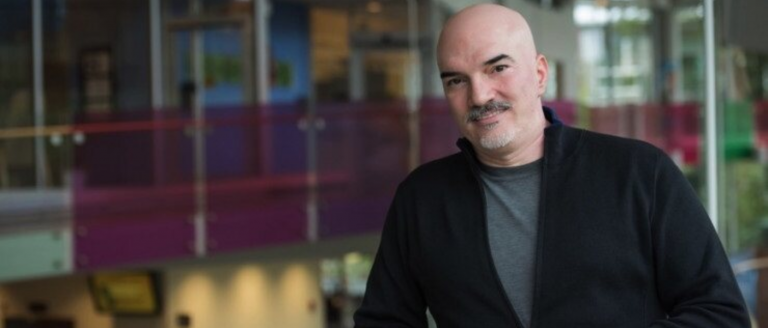
Dr. Babak Shadgan MD, MSc, PhD (Principal Investigator)
Assistant Professor, UBC Department of Orthopaedics, Division of Orthopaedic Research
Dr. Babak Shadgan is a Michael Smith Foundation for Health Research (MSFHR) Scholar, an assistant professor in the Department of Orthopaedics at the University of British Columbia (UBC), a faculty member at the UBC School of Biomedical Engineering, and a principal investigator at the International Collaboration on Repair Discoveries (ICORD), where he is directing the Implantable Biosensing Laboratory. With a medical degree in sports medicine from the University of London (U.K.), Dr. Shadgan earned his PhD in muscle biophysics from UBC. He completed an AO/ASIF Fellowship in Osteosynthesis at the Center for Diagnosis and Out-Patient Surgery, Freiburg, Germany, and a fellowship on NIRS-Diffused Optical Tomography at Martinos Center for Biomedical Imaging at Harvard University. His post-doctoral fellowship at UBC was focused on remote optical monitoring of muscle dysfunction in people with spinal cord injury.
In over two decades of medical practice and research, he has developed a specific knowledge in clinical biophotonics with a unique integrated approach. His current research is focused on the design and development of transcutaneous and implantable biosensors and interventions for evaluation and continuous monitoring of skeletal muscles, the spinal cord, free tissue flaps, and internal organ hemodynamics, metabolism, and function. He is also actively designing and developing novel wearable biosensor technologies and their applications in orthopedics and sports medicine.
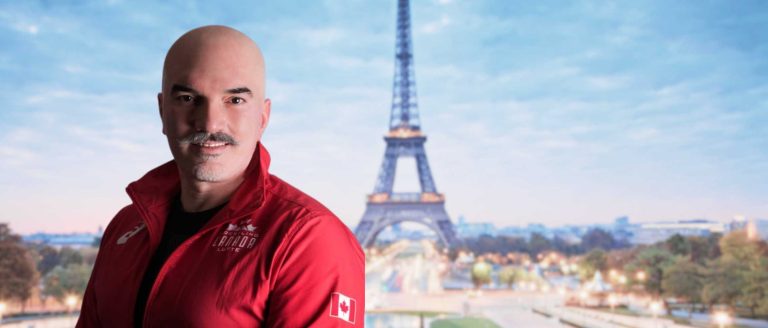
Dr. Pierre Guy MD, FRCSC (Co-Principal Investigator)
Professor, UBC Department of Orthopaedics, Division of Orthopaedic Trauma
Dr. Pierre Guy is a professor and clinician-scientist with the UBC Department of Orthopaedics, where he heads the Division of Orthopaedic Trauma. He completed his medical training and residency at McGill University and his orthopaedic trauma fellowships in Hannover and Berlin, Germany and at UBC. Dr. Guy also holds a master’s degree (MBA) from the John Molson School of Business, Concordia University. He is a practicing orthopaedic trauma surgeon at BC’s level 1 Trauma Centre, Vancouver General Hospital. He is a founding member of the Canadian Orthopaedic Trauma Society and an active member of the Canadian Orthopaedic Association and the Orthopaedic Trauma Association.
Dr. Konrad Salata MD, PhD, FRCSC (Co-Principal Investigator)
Clinical Instructor, UBC Department of Surgery, Vascular Surgery
Yekta Saremi BsKin (Research Assistant)
Shadgan Lab, ICORD
Mehdi Nourizadeh MD (MSc Candidate)
Shadgan Lab, ICORD
Learn more
- Canadian Orthopaedic Foundation Grant and award recipients
- 2024 Cy Frank Award Summary: Dr. Babak Shadgan and Dr. Pierre Guy
Noninvasive Optical Diagnosis of Chronic Exertional Compartment Syndrome
Latest News for Babak Shadgan and Pierre Guy
- UBC researchers awarded CIHR Project Grant to develop wearable sensor to detect sudden cardiac arrest conditions

- Dr. Babak Shadgan leads study exploring blood flow restriction training for strength building in people with spinal cord injury
- UBC Drs. Shadgan and Guy receive 2024–2025 Cy Frank Award for research on a non-invasive diagnostic method for lower leg chronic exertional compartment syndrome

- Dr. Babak Shadgan Appointed as a Medical Director in the 2024 Paris Olympic Games!